Prader-Willi Syndrome (PWS) is a rare genetic disorder that affects many aspects of a
child’s health, including growth, metabolism, muscle tone, and the musculoskeletal
system. Children with PWS often have low muscle tone (hypotonia) from birth and face
unique challenges such as developmental delays and excessive weight gain. In addition to
these well-known features, PWS is commonly associated with orthopedic issues –
especially involving the spine. As parents and families navigating a PWS diagnosis, it’s
important to understand the potential spine and orthopedic problems, how to monitor for
them, and the treatment options available. With specialized pediatric orthopedic care,
careful patient selection for interventions, and a compassionate, team-based approach,
children with PWS can achieve improved mobility and successful outcomes.
Orthopedic Challenges in PWS: Why Spine Issues Occur
PWS is characterized by severe hypotonia (low muscle tone) in infancy, which gradually
improves but never fully normalizes. This muscle weakness means the spine doesn’t have
typical muscular support, making children with PWS prone to developing scoliosis, an
abnormal curvature of the spine. In fact, scoliosis is present in a large proportion of
children with PWS – studies indicate anywhere from about 30% up to 70% or more of
patients may develop scoliosis. The curvature often starts early in life (some PWS infants
and toddlers show signs of scoliosis by age 2-4) and can progress during rapid growth
phases like adolescence. Low muscle tone allows the spine to bend sideways more easily,
and if a child with PWS is also overweight (common in PWS due to hyperphagia), the
added weight can strain the spine further. Besides scoliosis, kyphosis (forward rounding
of the upper back) can appear in later childhood or adulthood. Ligamentous laxity (loose
ligaments) in PWS may contribute to abnormal spinal alignment as well. Another factor
is the use of growth hormone therapy – many children with PWS receive growth
hormone to improve height, muscle mass, and metabolism. There has been some debate
about whether growth hormone might trigger or worsen scoliosis. Fortunately, research
shows that the incidence of scoliosis in PWS is not significantly increased by growth
hormone use. This is reassuring for families using this important therapy, though regular
spine monitoring remains critical. Overall, the combination of hypotonia, body
composition, and other PWS-related factors creates a “perfect storm” for spinal curvature
problems. Families and primary care providers should be aware of this risk so that regular
spine check-ups (at least annually) are part of the care plan.
Scoliosis in PWS: Early Detection and Monitoring
Scoliosis (a sideways curvature of the spine) is a major concern for patients with PWS, so
proactive monitoring is essential. Because scoliosis can develop very early in PWS,
pediatricians and parents should be on the lookout even in infancy and toddler years.
Many experts recommend a systematic spine examination at least once a year for children
with PWS. In practical terms, this means checking your child’s back for any asymmetry:
is one shoulder higher, one shoulder blade more prominent, or does the spine look
curved? If any doubt exists, a referral to a pediatric orthopedic specialist for a detailed
evaluation is warranted. Early detection is important because mild curves are easier to
manage and can often be treated with less invasive methods. According to data from a
large study, the median age when scoliosis is first noted in PWS was around 4.5 years.
Two peak periods for scoliosis progression in PWS are early childhood (around 5 years
old) and adolescence during the pubertal growth spurt. Knowing this, our clinic
emphasizes close observation during these high-risk windows. If a curve is detected, the
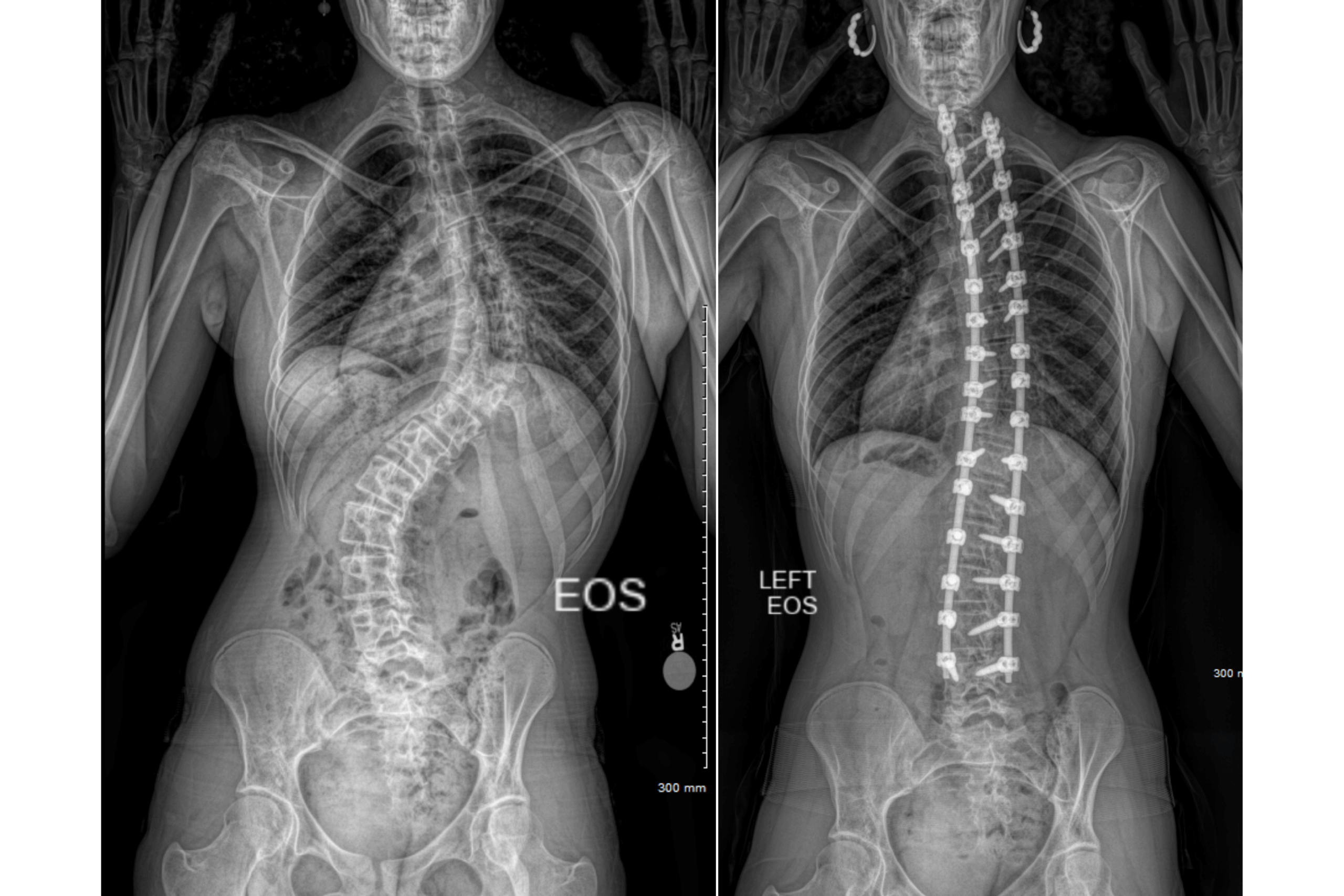
orthopedic team will likely obtain standing spine X-rays (to measure the Cobb angle,
which quantifies the curve). For very young children (infants/toddlers) who can’t easily
get X-rays, a physical exam or ultrasound might be used to assess the spine until they’re a
bit older. Families should also watch for signs like an unusual sitting posture or leaning to
one side – since PWS children often have delayed motor milestones, subtle changes in
posture during sitting or walking can be clues. It’s important to note that scoliosis in PWS
isn’t just a cosmetic or orthopedic issue; it can impact respiratory function. Because
children with PWS may already have breathing weaknesses (due to hypotonia and
sometimes obesity), a significant spinal curve can restrict lung expansion. Indeed, severe
kyphoscoliosis in PWS has been linked to respiratory failure and cor pulmonale (strain on
the heart from lung issues). This underlines why timely care of spinal issues is critical – a
well-aligned spine contributes to better breathing and overall health for a child with PWS.
Treatment Approaches for Spinal Curvature
When it comes to treating scoliosis in PWS, the approach is highly individualized, taking
into account the child’s age, the severity of the curve, and their overall health status.
Conservative (non-surgical) management is the first line for most children, especially
younger ones. For instance, if a toddler or preschooler with PWS has a moderate curve
(say 20–30 degrees), our specialists may recommend serial casting. In this technique,
performed under anesthesia, we gently manipulate the child’s spine towards straighter
alignment and apply a specialized cast from shoulders to hips. The cast holds the spine in
a corrected position, and over 2–4 months the child’s growth can help “remold” the spine.
Casts are changed periodically (every 2–4 months) as the child grows. This method has
shown encouraging results – about one in three young PWS patients in one series had
their scoliosis significantly improve with casting, allowing them to transition to a brace
thereafter. The goal is to guide the spine’s growth and delay or even avoid surgery while
the child is very small. After casting, or for milder curves, bracing is commonly used. A
thoracolumbar sacral orthosis (TLSO), which is a custom-molded plastic brace, can be
worn typically 16–20 hours a day to hold the spine and prevent further curvature. In
PWS, bracing is often started after a period of casting or if a curve is caught early.
Families sometimes worry that bracing could be uncomfortable or interfere with daily
life, but modern braces are fairly lightweight, and kids can do most activities in them. It’s
important to make bracing fun – we often decorate braces with child-friendly designs and
stress that wearing the brace is a team effort to “make my back strong.” For older
children or more severe scoliosis (curves exceeding ~40–50°), surgery may become
necessary. Surgical correction typically involves spinal fusion, where the surgeon
straightens the spine and fuses the vertebrae in place with rods and screws. However,
children with PWS require extremely careful surgical planning and specialized expertise.
Patient selection for surgery is critical – the surgeon, anesthesiologist, and the family
must weigh the benefits (a straighter spine, better sitting balance, potentially improved
breathing) against the risks. PWS patients have a higher risk of surgical complications than
typical scoliosis patients. Some reported complications include difficulties with
wound healing, higher chance of spine bone fusion not healing properly
(pseudoarthrosis), or even rare neurological issues. Furthermore, PWS children often
have increased skin picking behaviors and a high pain threshold, which can affect
recovery and wound care. At our pediatric orthopedic center, we mitigate these risks by
meticulous pre-operative preparation (including nutrition and respiratory optimization),
and engaging a multidisciplinary team for aftercare (such as endocrinologists for
hormonal support and pulmonologists for breathing support). In certain cases, newer
surgical techniques can be considered: for example, expandable growing rods for younger
children (to allow the spine to keep growing after surgery), or vertebral body tethering
(VBT) which is a fusionless surgery that preserves motion (though VBT is typically
reserved for idiopathic scoliosis and requires careful consideration in PWS due to
hypotonia). The bottom line is that if surgery is indicated, having it done at a center
familiar with rare diseases like PWS and neuromuscular scoliosis is crucial for safety and
success. The encouraging news is that with the right approach, many children with PWS
who undergo scoliosis treatment (whether casting, bracing, or surgery) do very well.
Families often report that after treatment, their children sit straighter, have improved
endurance, and in some cases improved lung function because the spine is better aligned.
Successful outcomes are most likely when problems are caught early and managed by an
experienced team.
Beyond the Spine: Other Orthopedic Issues in PWS
While spine issues are a major focus, PWS can affect other parts of the musculoskeletal
system too. Another common issue is hip dysplasia – an instability or shallow
development of the hip joint. Due to low muscle tone, some infants with PWS are born
with hip dysplasia or even dislocations. About 30–40% of children with PWS show
evidence of hip dysplasia on exams or X-rays. The good news is that serious hip
deformities requiring surgery are relatively uncommon, occurring in maybe 5% of
patients (around 1 in 20 children with PWS). Often, if a PWS baby has mild hip
dysplasia, we may adopt a conservative approach (like soft bracing) and monitor it,
because interestingly, adults with PWS do not seem to suffer the typical arthritis from
residual hip dysplasia that others would. However, any infant with PWS should have hip
screening and, if needed, treatment early – usually with methods like a Pavlik harness or
casting if the hip is dislocated. Flat feet (pes planus) are also frequently seen in PWS.
Low muscle tone leads to less support of the arches, so many toddlers with PWS develop
very flat, flexible feet. Without intervention, they could grow into adults with foot pain
due to misalignment. Our clinic’s approach is to use custom orthotic inserts or small
braces (UCBL orthoses) in early childhood to shape the foot’s arch and heel alignment.
These are usually worn during the day inside shoes. By providing proper foot alignment
while a child is growing, we help them develop a more typical arch and improve their
walking efficiency. Most kids with PWS tolerate these inserts well, especially if we start
them when the child is first learning to walk, as it just becomes a normal part of their
routine. Another aspect to be aware of is osteoporosis and fractures. Children and
adolescents with PWS have an increased risk of low bone density. Contributing factors
include reduced muscle forces on bones, less mobility in some cases, and nutritional
differences. Some studies report that up to 20–30% of kids with PWS have had fractures due
to osteopenia (brittle bones). Parents should ensure their child has adequate calcium
and vitamin D, and endocrinologists sometimes check bone density in PWS patients,
especially if there’s a history of fractures. Weight-bearing activities (supervised exercise,
walking) can strengthen bones, and newer treatments like bisphosphonates have been
used in severe cases to improve bone density. Preventing fractures also circles back to
treating scoliosis – a very twisted spine can itself be at risk for vertebral fractures. Whole-
child care means we address nutrition, bone health, and physical therapy in conjunction
with any orthopedic treatments.
Compassionate, Specialized Care Leads to Success
Caring for a child with PWS requires a team approach, and families should feel that they
are not alone on this journey. At our pediatric orthopedic practice, we work closely with
geneticists, endocrinologists, nutritionists, pulmonologists, and therapists to support
every aspect of the child’s health. We understand that parents of children with PWS often
face additional stressors – concerns about their child’s future, questions about surgical
risks, and juggling multiple therapies. Our role is not only to provide surgical and
medical expertise but also to offer guidance, support, and empathy. For example, if a
brace is needed for scoliosis, we take the time to explain to both parent and child why it’s
important and how it will help them do the things they love, like playing or sitting
comfortably in class. Because PWS is a rare disease, many local providers may have
limited experience in its orthopedic management. We frequently provide second opinions
for families – perhaps your local doctor has recommended a spine surgery and you feel
unsure, or you want to confirm the best course of action for a hip problem. Seeking a
second opinion at a specialized center is a wise step; we can often either reassure you that
the plan is sound or suggest alternative approaches tailored to PWS. We also welcome
families traveling from other regions or even countries (“medical tourism”) when
specialized care is not available near home. Our practice is accustomed to coordinating
with out-of-town families to make the process as smooth as possible, recognizing the
extra effort it takes for you to come to us for expert care. In summary, Prader-Willi
Syndrome comes with significant orthopedic challenges, especially involving the spine,
but there is hope and help available. Through vigilant monitoring, early interventions like
casting and bracing, and judicious use of surgery in the right cases, children with PWS
can maintain better alignment and function. We have seen children with PWS go from
struggling to sit due to a severe scoliosis, to post-treatment sitting upright with a big
smile and engaging more with their world. Every child with PWS is unique, and our
commitment is to provide compassionate, individualized care that maximizes their health
and abilities. With careful patient selection for any procedure and a focus on safety, we
strive for successful outcomes that improve quality of life. Families can take comfort in
knowing that with specialized pediatric orthopedic support, many PWS-related
orthopedic issues can be managed effectively – allowing your child to focus on being a
child, growing, learning, and enjoying life to the fullest extent possible.
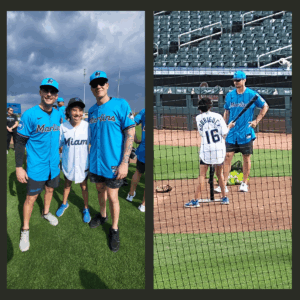
Watch the video to see how life-changing the right orthopedic care can be.
If you have concerns about your child’s spinal health or would like to schedule a consultation, contact Dr. Arun Hariharan’s office today. Early intervention can make all the difference for your child.